The Student Engineer Behind a New Era of Healthcare Clear Prices, Clear Labs, No Surprises
In the American healthcare system there is a simple but brutal scenario. A person comes to the hospital, goes through tests and procedures, then waits for weeks for a letter from the insurance company and only then finds out how much the visit actually cost. For many people this hits not only their health but also their wallet.
Gavkhar Abdukarimova, a graduate student in Health Information Management at Lewis University in Illinois, has decided it is time to end this scenario. She is not a doctor and not an insurance broker. She is a person who understands data, laws, and information systems. And her goal is simple: to make sure the patient sees an honest estimate of their potential expenses before they step through the hospital door.
In her research project, Gavkhar developed the architecture of a HIM platform with a telling name: A Secure HIM Platform for Hospitals: Telegram-Style Security, AI Triage, and Cost Pre-Calculation. This is not an abstract startup idea but a detailed blueprint of how a hospital information system should work so that it simultaneously protects medical data, helps clinicians, and calculates the money for the patient in advance.
First comes security. Gavkhar takes as a foundation the principles of highly secure messengers: minimization of metadata, short sessions, device binding, instant blocking of access tokens. She transfers this philosophy into healthcare, adding what developers usually forget about: a controlled break glass mechanism for emergencies, strict control over the purposes of data access, and an immutable audit of all staff actions. In Gavkhar’s system, a patient in their portal can see who opened their record, when, and for what reason, and this is not pretty marketing language but a mandatory part of the architecture.
The second layer is artificial intelligence. The platform does not turn the model into an all-knowing doctor. On the contrary, AI sits in a separate sandbox and does what burns clinicians’ time: it sorts incoming messages, gathers missing details, and suggests whether self service, an in person visit, lab work, or an urgent consultation is needed. All of this happens under strict HIPAA constraints, with filtering of personal data before and after processing and with a complete audit trail. The task of the AI is to offload clinicians, not to replace them or drag millions of lines of sensitive data into model logs.
A separate part of the project is devoted to how the patient sees their tests. If a person takes a lab test, the result on the platform does not look like a set of cryptic abbreviations and numbers. The system automatically breaks down each parameter, explains in simple words what exactly was measured, shows the normal range, and highlights what is decreased and what is elevated for this particular patient. Instead of a dry “elevated” flag, the patient receives a clear explanation of what this might mean and which questions should be discussed with the doctor. The same decoded data is automatically sent to the Family Medicine physician in their professional interface so they see the dynamics rather than just another pdf from the lab. The patient and the family doctor are finally looking at the same numbers and understanding them in the same way.
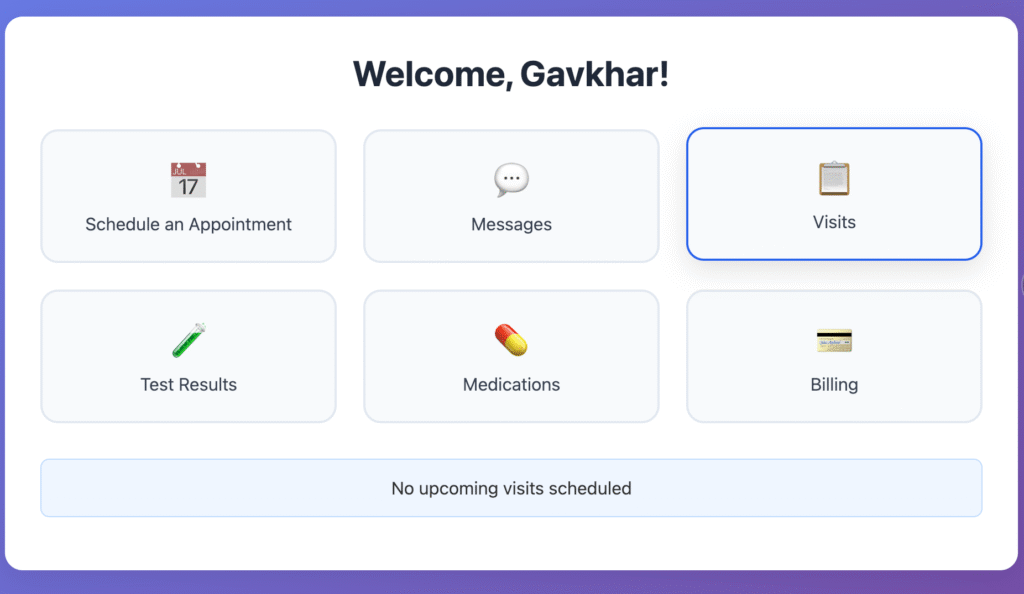
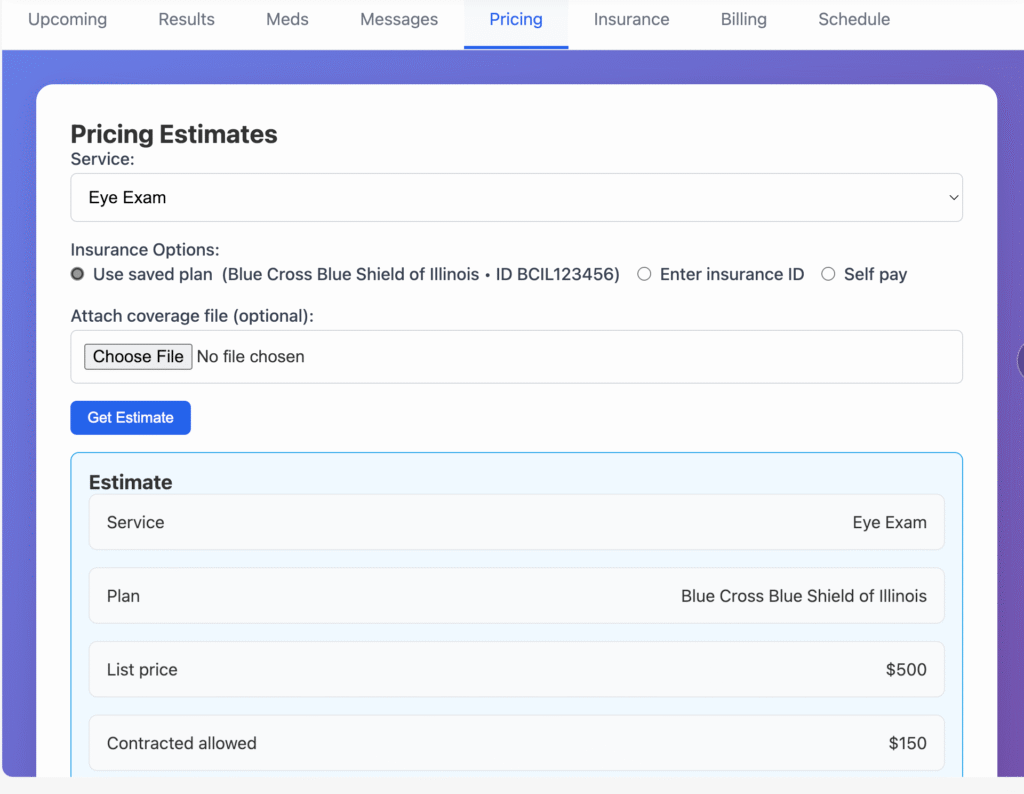
Next comes the financial module. It answers the question that usually remains unanswered: “How much will I pay?” The platform pulls machine readable rate files from insurers under Transparency in Coverage and from hospitals under Hospital Price Transparency, understands the difference between the professional and facility components of the bill, takes into account CPT modifiers, bundling rules, in network status, deductible, copays, coinsurance, and the out of pocket maximum. As a result, the patient sees a range of their expected financial responsibility and a confidence index for this estimate. For self pay patients, the system immediately generates a Good Faith Estimate in the logic of the No Surprises Act.
Roughly speaking, if earlier a patient walked into the exam room as if into a casino, in Gavkhar’s model they go in with a clear stake and transparent rules of the game. The goal is to achieve a mean absolute error of no more than 20 percent and to ensure that in 80 to 90 percent of cases the final bill falls within the range shown in advance. For the CFO this is a manageable risk. For the patient it is psychological and financial stability.
It is important that this whole story does not live in a vacuum. The platform is designed so as not to violate Information Blocking and TEFCA rules: data is not locked in a black box for the sake of security but is exchanged via FHIR and SMART on FHIR standards, with fine grained access control at the level of individual record fields. In essence, Gavkhar is proposing a mature cybersecurity model: minimum necessary access, maximum transparency, and zero theater.Behind the dry engineering lies a personal motivation. Gavkhar is originally from Uzbekistan, with a background in biology and experience working in an oncology center. She has chosen immuno oncology and quality of care as her long term theme and openly says that she wants to build a pediatric oncology hospital where high technology and human compassion stand side by side. For such a hospital, the patient’s money is not an abstract line in a spreadsheet but a factor that determines whether a child will reach treatment at all.
This is why her platform is not just another healthcare IT product. It is a building block in a future where the hospital shows the price in advance, the state demands transparency, patients understand their test results and treatment plan, and people stop fearing the bill as much as the diagnosis.
Today it is the work of a student and a research prototype. Tomorrow it can be the basis for a startup, a pilot in a health system, or the core of that very oncology hospital she dreams about. And if a new era of healthcare really starts with a simple thing – an honest answer to the questions “What is going on with my health?” and “How much will this cost?” before the patient walks into the exam room, it is quite possible that one of the people who launched this wave will be a student from Lewis University named Gavkhar Abdukarimova.

